MALARIA
Malaria is a protozoan (parasitic) infection caused by an infected Anopheles mosquito bite. About a quarter-billion infections occur annually, of which more than half million die each year. Malaria symptoms include high fever, body aches and rigors (intense shivering) with risks involving vital organs like your brain (causing confusion and coma), liver (jaundice), and kidneys (renal failure).
Travellers can get Malaria in most parts of Africa, Asia, Central and South America, the Caribbean and South Pacific.
Most travellers are not aware of such a risk and do not seek a pre-travel consultation.
Prevention:
- Do not let Mosquitoes bite you (See: Mosquitoes Safety).
- Take Chemoprophylaxis or anti-malarial drugs that your travel doctor will prescribe to you. These drugs differ according to your itinerary, health status and many other factors. Don’t worry, your travel doctor will give you the right one and tell you how to use it!
- Seek medical advice ASAP if you are symptomatic, even if you are taking anti-malarial drugs.
Malaria is serious! Always keep that in mind.
Self-Treatment:
- Your travel doctor may prescribe drugs for self-treatment in certain situations. This is different from Chemoprophylaxis. Talk to your travel doctor.
- Seek medical care immediately. Medications for self-treatment are not substitute for medical advice.
JET LAG
When you cross multiple time zones the rhythmic cues to the brain will alter some of the chemical signals that control the sleep-wake cycle. Its thought the Melatonin synthesis and release in the brain that is stimulated by darkness and suppressed by light, changes in a way that affects the internal body clock. This results in temporary sleep disturbance, which lasts longer with the more time zones traveled, especially eastward travel.
Eastward travellers will not be able to fall asleep at their destination’s routine bedtime and will have difficulty waking up in the morning. Westward travellers will have the opposite experience; they will fall asleep earlier and wake up earlier.
Prevention:
- Reset your body clock by doing a simple trick; go to bed 1-2 hours LATER than your usual bedtime for few days before WESTWARD travel. If intending to do EASTWARD travel go to bed 1-2 hours EARLIER for few days.
- Healthy diet and exercise.
- Seek light exposure at destination during the evening in westward travel. If you are traveling eastward the bright sun light will be a good stimulus to help you adjust your internal clock to the new environment.
- Avoid alcohol and caffeine.
- Don’t consume large meals, and drink plenty of water.
- Try to have a nap if your flight is long.
Self-Treatment:
Your travel doctor can give you a prescription for self-treatment medication to help you sleep well at your destination.
ALTITUDE ILLNESS
Altitude illness is comprised of three syndromes:
Acute Mountain Sickness (AMS): This is very common. Symptoms are headaches that usually start few hours after arriving at the high altitude, nausea, loss of appetite and fatigue.
High-Altitude Cerebral Edema (HACE): This is rare but fatal if person fails to descend after symptoms start. It’s like AMS plus lethargy, drowsiness, confusion and an unsteady gait. It can occur with HAPE.
High-Altitude Pulmonary Edema (HAPE): The symptoms include cough, breathlessness and exercise intolerance. Fatal if a person fails to descend immediately. Can occur with the other two syndromes.
The main reason for altitude illness syndromes is the hypoxia associated with heights of 1500 m (4900 ft) and higher.
High-altitude destinations are widely sought by many travellers and include Cuzco, Peru (3400 m; 11150 ft), La Paz, Bolivia (3780 m; 12400 ft), Lhasa, Tibet (3660 m; 1200 ft), Everest Base Camp, Nepal (5364 m; 17598 ft), and Kilimanjaro, Tanzania (5895 m; 19341 ft).
To experience the magic of the high-altitude destinations you need good preparation techniques and health advice from your travel doctor, since altitude illness syndromes (especially HACE and HAPE) are very serious.

Prevention:
- Early recognition of symptoms.
- Acclimatization: Done by gradual ascent, especially after reaching 2500 m altitude. It’s advisable to ascend no more than 500 m per day and spending an extra acclimatization day every 1000 m.
- Avoid alcohol.
- Your doctor will give you medications to help acclimatization and prevent altitude illness. Make sure to carry them in your backpack with clear labels and instructions.
- When going to high-altitude destinations ALWAYS purchase medical and evacuation insurance. (See: Before You Travel).
- Memorize the GOLDEN RULES OF ALTITUDE:
If you feel unwell at altitude, its altitude illness until proven otherwise.If you have symptoms of AMS, go no higher.If your symptoms are worsening (as with HACE or HAPE), you must go down immediately.Courtesy of Dr. David Shlim
Self Treatment:
- Immediate descent (See Above: The Golden Rules of Altitude).
- Call for help and notify your team leader.
- Take the appropriate self-treatment medication(s) prescribed by your travel doctor according to your symptoms. Follow the instructions on the medications bottles in your backpack. Make sure that your doctor gives clear,written instructions.
- Look for emergency medical care immediately.
- Call your evacuation insurance using a satellite phone.
MOTION SICKNESS
Prevention:
- Avoid alcohol and caffeine, drink plenty of water and avoid large meals.
- Sit near the wing of the aircraft or in a cabin if possible.
- Look at a fixed point in the horizon or close your eyes.
- Listen to music or use aromatherapy like mint or citrus scents.
- Pop in a lozenge, preferably ginger flavoured.
Self-Treatment:
- Ask your travel doctor to prescribe you a self-treatment medication that is suitable for your age and health status.
- Seek medical advice if available or when you arrive at your destination.

TRAVELLERS’ DIARRHEA (TD)
TD affects millions of travellers visiting Asia, Africa, South America and the Caribbean. 1-3 out of 4 travellers will have TD.
Travellers Diarrhea is mainly caused by bacterial infection (sometimes viral or protozoan) of the gastrointestinal tract by ingesting contaminated food and drinks.
Symptoms may include diarrhea, vomiting, fever, and abdominal cramps or sometimes bloody diarrhea.
TD has a great implication on travellers.
Imagine that you take a weeklong vacation to spend with your family on the beach and it gets ruined by TD.
Prevention:
- TD can be prevented by health advice and vaccine. Ask your travel doctor how. (See: Vaccines & Food and Water Safety sections for more information on TD prevention).
Treatment:
- Your travel doctor will give you a prescription for TD self-treatment.
- Hydration using ORS (oral rehydration solutions), or commercial sport drinks.
- Seek medical advice ASAP.
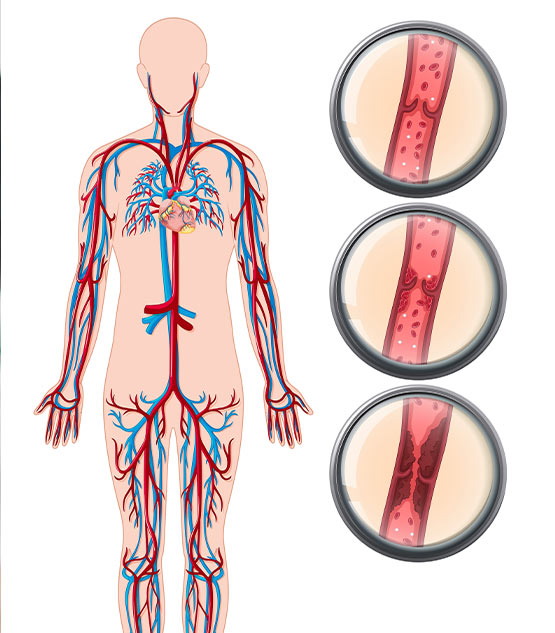
DEEP VEIN THROMBOSIS AND PULMONARY EMBOLISM
Prevention:
- Try to sit in an isle seat in the aircraft (if feasible). This will make it easier for you to move around (if the seatbelt sign is off) and exercise calf muscles. If you can’t move out of the seat you should perform calf exercises. Ask your travel doctor to show you how.
- Visit your travel doctor before intended travel. Your travel doctor will assess if you have risk factors and need prescription for compression stockings and or special prophylactic medication.
- Taking baby aspirin and hydration will NOT prevent DVT associated with air travel.
There is NO self-treatment. It’s a MEDICAL EMERGENCY and you should seek immediate medical advice.